
Newly Approved Specialty Drugs Advance Care for Inflammatory and Autoimmune Diseases
Key Takeaways
- Specialty drugs comprised 80% of novel medication approvals in 2024, highlighting pharmacists' critical role in managing these therapies' impacts.
- Delgocitinib, a topical JAK inhibitor, is the first approved therapy for moderate-to-severe chronic hand eczema, offering significant improvements in skin clearance and quality of life.
- Prademagene zamikeracel, a gene therapy for recessive dystrophic epidermolysis bullosa, demonstrated substantial wound healing efficacy, despite high upfront costs.
- Dupilumab's new indications for chronic spontaneous urticaria and bullous pemphigoid expand its use, offering sustained remission and reduced corticosteroid requirements.
- Upadacitinib and guselkumab provide non-steroidal options for giant cell arteritis and Crohn disease, respectively, enhancing treatment flexibility and patient outcomes.
Approximately 80% of novel medication approvals in 2024 were specialty drugs.1 As medication experts, pharmacists are uniquely positioned to assess and manage the clinical and operational impacts of these therapies within their practice settings. From evaluating indications to navigating access challenges, pharmacy teams play a vital role in supporting both providers and patients as new products enter the market.
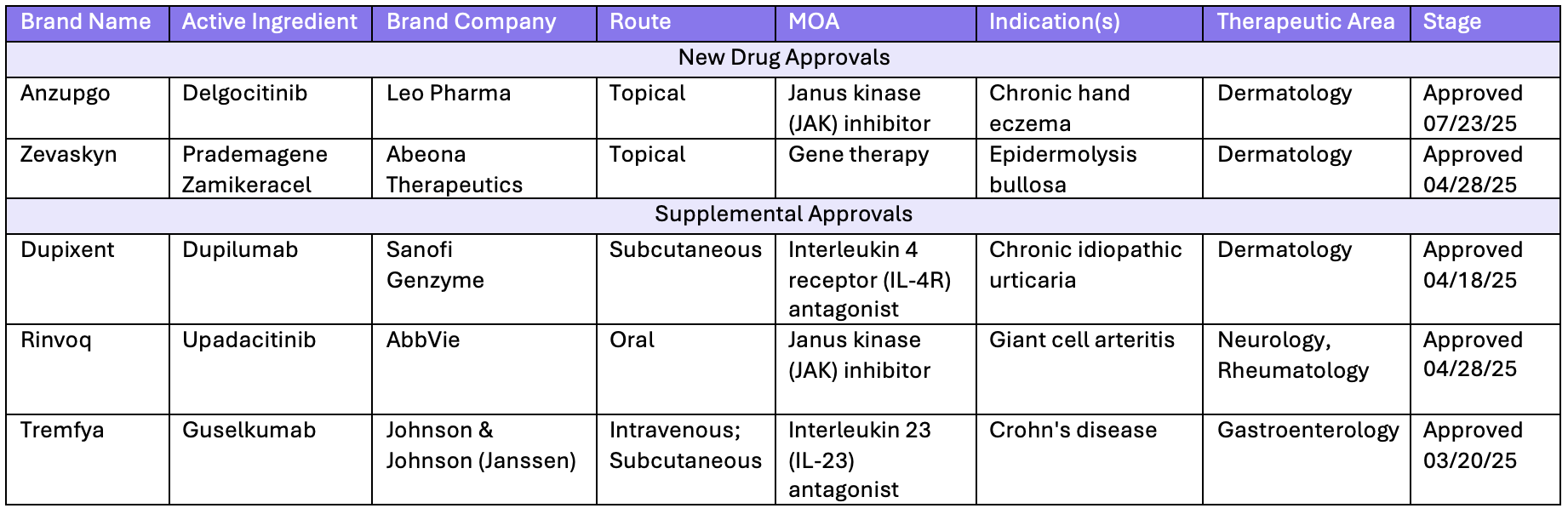
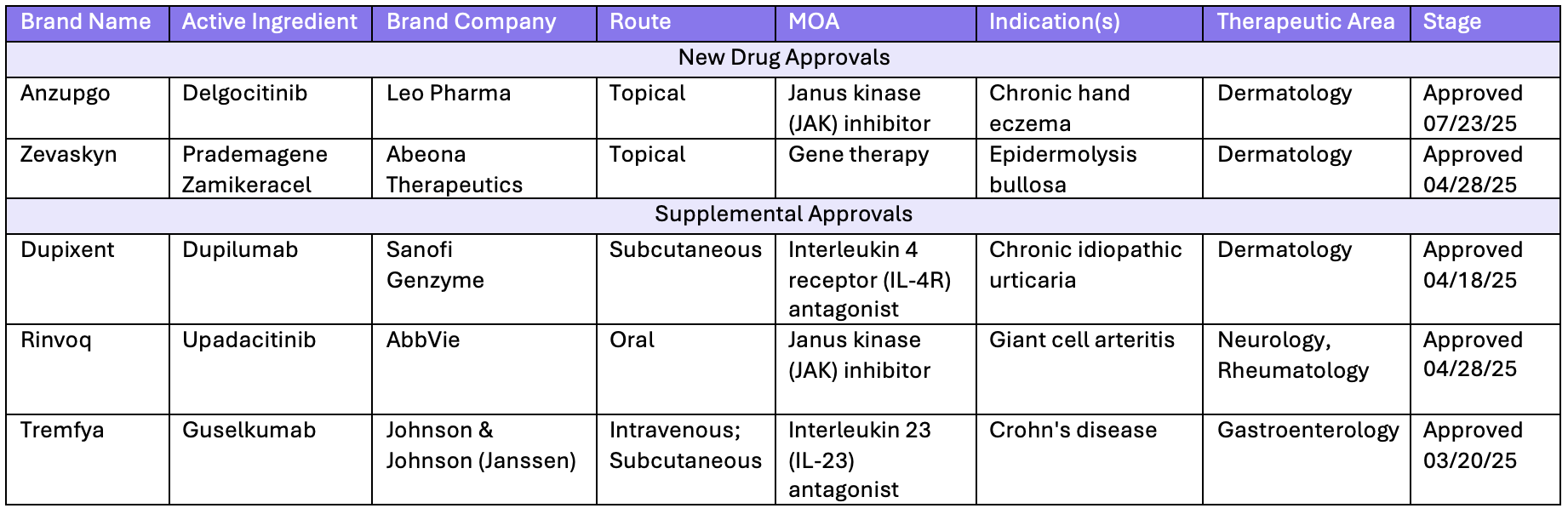
In 2025, there were several approvals of novel therapies and new supplemental indications in the specialty pharmacy space.

Inflammatory and Autoimmune Conditions
Inflammatory conditions are characterized by inflammation as a response to the immune system or triggers.2 Autoimmune disorders cause inflammation when the body’s immune system attacks its own healthy tissues.3 These conditions include disorders across multiple specialties, such as rheumatology, gastroenterology and dermatology. Recent therapeutic approvals have changed treatments for immune-mediated and inflammatory conditions including eczema, epidermolysis bullosa, chronic spontaneous urticaria, bullous pemphigoid, giant cell arteritis and Crohn disease.
Topical Therapy for Chronic Hand Eczema
Delgocitinib (Anzupgo; LEO Pharma) is a topical Janus kinase (JAK) inhibitor approved for the treatment of moderate-to-severe chronic hand eczema (CHE) in adults who have had an inadequate response to topical corticosteroids or for whom corticosteroid therapy is not appropriate.4 It is the first and only approved therapy specifically indicated for adults with moderate-to-severe CHE. CHE is hand eczema persisting for more than 3 months or recurring at least twice within 1 year.5
Clinical trials leading to FDA approval of delgocitinib demonstrated rapid and substantial improvements in skin clearance, significant relief from itch and pain, and a favorable safety profile comparable to that of the vehicle cream.6 The recent approval of delgocitinib offers a promising new therapeutic option and has the potential to significantly improve outcomes and quality of life for patients affected by moderate-to-severe forms of the disease.
Gene Therapy Treatment for Recessive Dystrophic Epidermolysis Bullosa
Prademagene zamikeracel (Zevaskyn; Abeona Therapeutics) is a topically administered gene therapy approved for the treatment of recessive dystrophic epidermolysis bullosa (RDEB), representing the third FDA-approved therapy for epidermolysis bullosa (EB).7 Previously approved treatments are beremagene geperpavec-svdt (Vyjuvek; Krystal Biotech), another topical gene therapy, and birch triterpenes (Filsuvez; Chiesi USA), a topical gel formulation.
RDEB is a severe form of EB, a rare, inherited connective tissue disorder characterized by defects in epidermal-dermal cohesion. This results in extremely fragile skin, leading to blistering, chronic nonhealing ulcerations, and scarring in response to minor trauma or friction.8 In clinical trials, prademagene zamikeracel demonstrated a 50% or better wound healing response in 81% of treated patients, compared to only 16% in the control group. Although the upfront cost is substantial at $6.2 million for 2 treatment cycles,prademagene zamikeracel’s clinical efficacy suggests potential long-term cost-effectiveness by reducing the need for long-term therapy.9
Biologic Treatment for Chronic Spontaneous Urticaria and Bullous Pemphigoid
Dupilumab (Dupixent; Sanofi, Regeneron) has received FDA approval for the treatment of chronic spontaneous urticaria (CSU) and bullous pemphigoid. CSU is a condition characterized by the presence of hives on most days for a duration of at least 6 weeks.11 It is the second biologic approved for this indication alongside omalizumab (Xolair; Genentech, Novartis). Clinical studies showed that dupilumab was effective in patients naïve to omalizumab, though it did not demonstrate significant efficacy in those who had previously failed omalizumab therapy.10
Bullous pemphigoid is the most common autoimmune subepidermal blistering disorder, typically characterized by the development of tense blisters and severe, generalized pruritus.12 Dupilumab offers the potential for sustained disease remission and significant reduction in pruritus by targeting the type 2 immune response underlying bullous pemphigoid. In clinical trials, treatment with dupilumab resulted in a higher proportion of patients achieving sustained remission, greater improvements in itch severity, and a reduced cumulative requirement for oral corticosteroids compared to standard therapy.14 These new indications expand upon dupilumab's existing approved uses in other inflammatory and allergic conditions.
Non-Steroidal Treatment for Giant Cell Arteritis
Upadacitinib (Rinvoq; AbbVie) has been approved for the treatment of giant cell arteritis (GCA), a chronic inflammatory vasculitis that primarily affects large- and medium-sized arteries.15 This new indication expands upadacitinib’s approved uses beyond its existing indications for other inflammatory conditions, including rheumatoid arthritis and ankylosing spondylitis. Clinical trials resulted in sustained remission with substantial steroid reduction in patients using upadacitinib.17 As an alternative to long-term corticosteroid use in this patient population, upadacitinib offers an effective therapeutic option. Given the substantial adverse effect profile associated with chronic steroid use,upadacitinib represents meaningful advancements in GCA management.Upadacitinib offers an alternative non-steroidal therapy for the treatment of giant cell arteritis, alongside tocilizumab (Actemra; Genentech), which is also approved for this condition.
Subcutaneous Regimen for Severe Crohn Disease
Guselkumab’s (Tremfya; Johnson & Johnson) new indication for the treatment of moderate to severe Crohn disease introduces an additional therapeutic option targeting the IL-23 pathway.19 In clinical trials leading to its approval, guselkumab demonstrated significant efficacy, with patients in the treatment groups achieving both clinical remission and endoscopic response.20 Crohn disease management has advanced throughout the years, but many patients continue to experience symptoms that greatly impact their quality of life. The availability of new therapeutic treatments for these patients presents more options to achieve desired outcomes.21,22 The availability of a fully subcutaneous regimen provides increased flexibility and convenience for patients and health care providers.
Pharmacists’ Vital Role
Specialty medications require special handling, storage, dispensing, monitoring, and payor coverage. When a new medication becomes available to a health system, pharmacists help to meet these requirements, whether it's related to clinical monitoring criteria, health plan requirements, copay assistance, or medication education. Pharmacists help mitigate future emergency department visits and inpatient stays and reduce unnecessary adverse events and readmissions. They also help health systems avoid unnecessary costs by providing follow-up care to make sure patients are monitored for symptoms and take their medications on time. These high-touch services aim to make it easy for providers and patients to access specialty pharmaceuticals in the safest, most effective and convenient way possible.
Pharmacists are dedicated to ensuring patient access to transformative specialty therapies. With the release of new medications, expansion of indications, and approval of new formulations, there is significant potential to enhance both patient outcomes and access. Experienced teams collaborate closely with health care providers to minimize barriers, ensuring patients receive critical therapies. Additionally, they can assess the financial impact of new treatments to support informed business decisions. Whether coordinating with manufacturers to acquire new medications, managing prior authorizations, or delivering essential clinical insights to patients and providers, the commitment to patient care remains at the forefront of a pharmacist’s role.
REFERENCES
- Novel drug approvals for 2024. FDA. Updated July 14, 2025. Accessed November 19, 2025. https://www.fda.gov/drugs/novel-drug-approvals-fda/novel-drug-approvals-2024
- Chen L, Deng H, Cui H, et al. Inflammatory responses and inflammation-associated diseases in organs. Oncotarget. 2018;9:7204-7218. doi:10.18632/oncotarget.23208
- Autoimmune disease. National Cancer Institute. Accessed November 19, 2025. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/autoimmune-disease
- Anzupgo (delgocitinib) cream is now the first and only FDA-approved treatment for moderate-to-severe chronic hand eczema (CHE) in adults. News release. BusinessWire. July 23, 2025. Accessed November 19, 2025. https://www.businesswire.com/news/home/20250723115252/en/ANZUPGO-delgocitinib-Cream-Is-Now-the-First-and-Only-FDA-Approved-Treatment-for-Moderate-to-Severe-Chronic-Hand-Eczema-CHE-in-Adults
- Ghezzi G, Falcidia C, Paolino G, et al. Chronic hand eczema (CHE): a narrative review. Derm Ther. 2025;15:771-795. doi:10.1007/s13555-025-01365-7
- Anzupgo [prescribing information]. LEO Pharma, Inc; July 2025. Accessed November 19, 2025. https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/219155s000lbl.pdf
- Zevaskyn [prescribing information]. Abeona Therapeutics Inc; April 2025. Accessed November 19, 2025. https://www.fda.gov/media/186511/download
- Soro L, Bartus C, Purcell S. Recessive dystrophic epidermolysis bullosa: a review of disease pathogenesis and update on future therapies. J Clin Aesthet Dermatol. 2015;8(5):41-46.
- US FDA approves Zevaskyn (prademagene zamikeracel), the first and only cell-based gene therapy for patients with recessive dystrophic epidermolysis bullosa (RDEB). News release. Abrona Therapeutics. April 29, 2025. Accessed November 19, 2025. https://investors.abeonatherapeutics.com/press-releases/detail/303/u-s-fda-approves-zevaskyn-prademagene-zamikeracel
- Dupixent [prescribing information]. Regeneron; June 2025. Accessed November 19, 2025. https://www.regeneron.com/downloads/dupixent_fpi.pdf
- Hsieh J, Lee JK. Chronic spontaneous urticaria. CMAJ. 2017;189(2):E77. doi:10.1503/cmaj.150951
- Baigrie D, Nookala V. Bullous Pemphigoid. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Accessed November 19, 2025. https://www.ncbi.nlm.nih.gov/books/NBK535374/
- Zhao L, Wang Q, Liang G, et al. Evaluation of dupilumab in patients with bullous pemphigoid. JAMA Dermatol. 2023;159(9):953-960. doi:10.1001/jamadermatol.2023.2428
- Results With Dupixent. Dupixent. Accessed November 19, 2025. https://www.dupixent.com/bullous-pemphigoid/about-dupixent/results-with-dupixent
- Maz M, Chung SA, Abril A, et al. 2021 American College of Rheumatology/Vasculitis Foundation guideline for the management of giant cell arteritis and Takayasu arteritis. Arthrit Rheumatol. 2021;73(8):1349-1365. doi:10.1002/art.41774
- Rinvoq [prescribing information]. AbbVie Inc; October 2025. Accessed November 19, 2025. https://www.rxabbvie.com/pdf/rinvoq_pi.pdf
- Durable Remission With Rapid Steroid Reduction. Rinvoq. Accessed November 19, 2025. https://www.rinvoqhcp.com/giant-cell-arteritis/efficacy
- Ameer MA, Vaqar S, Khazaeni B. Giant cell arteritis (temporal arteritis). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Accessed November 19, 2025. https://www.ncbi.nlm.nih.gov/books/NBK459376/
- Tremfya [prescribing information]. Janssen Biotech, Inc; September 2025. Accessed November 19, 2025. https://www.jnjlabels.com/package-insert/product-monograph/prescribing-information/TREMFYA-pi.pdf
- Why choose Tremfya? Tremfya. Accessed November 19, 2025. https://www.tremfya.com/crohns-disease/results/
- Feuerstein JD, Ho EY, Shmidt E, et al. AGA clinical practice guidelines on the medical management of moderate to severe luminal and perianal fistulizing Crohn’s disease. Gastroenterol. 2021;160(7):2496-2508. doi:10.1053/j.gastro.2021.04.022
- US FDA approves Tremfya (guselkumab), the first and only IL-23 inhibitor offering both subcutaneous and intravenous induction options, for adult patients with moderately to severely active Crohn’s disease. News release. Johnson & Johnson. March 20, 2025. Accessed November 19, 2025. https://www.jnj.com/media-center/press-releases/u-s-fda-approves-tremfya-guselkumab-the-first-and-only-il-23-inhibitor-offering-both-subcutaneous-and-intravenous-induction-options-for-adult-patients-with-moderately-to-severely-active-crohns-disease
