An Unwelcome Cashflow Strain on Hospitals: 340B Rebate Model Program Impact

By Clearway Health
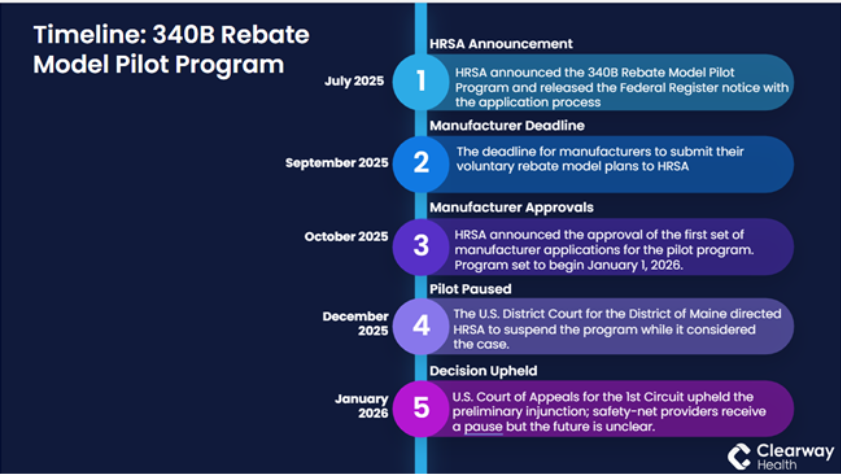
On December 31, 2025, A federal judge ordered a pause on the launch of the Health Resources and Services Administration’s (HRSA) 340B Rebate Model Pilot Program, which was scheduled to begin on January 1, 2026. The American Hospital Association, along with the Maine Hospital Association and four safety-net hospitals, filed a suit on December 1, 2025 to block the program. The judge ordered a preliminary injunction, noting the federal program would likely violate the Administrative Procedure Act.
The U.S. Court of Appeals for the 1st Circuit upheld that preliminary injunction on January 7, 2026. On January 12, 2026, the federal government announced it would drop its appeal of Judge Walker’s order blocking implementation of the Pilot Program and return it back to HRSA for reconsideration. While safety-net providers received a pause from the controversial plan to replace discounts with rebates under the 340B Drug Pricing Program, they are still not in the clear.
Clearway Health recently hosted a Becker’s webinar on the ‘Unwelcome Cashflow Strain on Hospitals: 340B Rebate Model Program Impact’ with Allison Arant, senior vice president, client development and marketing for Clearway Health serving as the moderator along with three panelists:
- Beth Feldpush, senior vice president, policy and advocacy, America's Essential Hospitals
- Shannon Sale, executive vice president, chief administrative officer, Grady Health System
- Nicole Faucher, MS, president, Clearway Health
The webinar addressed important questions impacting safety-net hospitals across the country regarding the potential impact of the 340B rebate model on cashflow strain. Please note that the webinar was recorded before the pilot was paused.
Question and Answer:
Q: What’s happened over the last seven months to get us to where we are now with the 340B Rebate Model Pilot Program?
Beth Feldpush: What was absent from HRSA's notice in October were the safeguards for how this financially impactful program should be run. For example, if a hospital or community health center is concerned that they have not gotten the rebate in a timely manner from a manufacturer, the only guidance HRSA gives is to email the general inbox at HRSA and ask for the rebate. There's a lot around this pilot program that remains very much in question. Manufacturers have been told they need to give hospitals their rebates within 10 days of a hospital submitting a claim, but there are no safeguards to ensure they are upholding this practice.
Q: What makes this such a significant change for hospitals; does it create a precedent for similar models in healthcare?
Shannon Sale: At Grady Health System, the 340B changes were abrupt; they came right in the middle of budgeting season while we were preparing for 2026. We needed to reevaluate our pharmacy budget inputs to look at what the financial impact was going to be, particularly on our cashflow. Our initial estimate is that we were going to have an upfront expense of $35 million that the rebate program would ideally pay back. We prepared for this change on two fronts. First, we put all the workflows in place that would help us understand what the numbers were going to be. We signed up for Beacon to access the new rebate model platform for 340B claims.
We recognize there have been other pilot [programs] along the way, but at this magnitude and timing from October to the beginning of the year was an extremely quick turnaround. Second, determining how to manage the upfront impact of $35 million is monumental for us, as it is for other hospitals and health systems, along with what steps to take to offset this impact.
Nicole Faucher: We spend a lot of time looking at the processes, data and analytics required to help set the stage for 340B resiliency. Over the last few years, we have all faced changes whether it's around contract pharmacy restrictions, various manufacturer restrictions -- and this adds another layer. The reality is the 340B Program has grown significantly related to its overall value to the system, and the manufacturers continue to have concerns around diversion or duplicate discounts.
We need to prepare ourselves for increased transparency and visibility that are the underpinnings of this new model. It will certainly have implications for capital planning in the organizations we work with. We are looking at building new operational processes in an uncertain time, and we are considering the administrative costs hospitals will need to implement to manage the program. When you compound the financial benefit in a rebate model versus the upfront discount, it creates a completely different process, where this becomes an accounts receivable situation versus the discount.
Shannon Sale: We see this as a significant change and a fundamental shift from the original intent of the 340B Program, which is a federal program that allows certain hospitals to receive discounted prices for outpatient drugs to improve access for needed medications to patients who would otherwise not be able to afford them.
Through this program, we already have eligibility criteria, program requirements and detailed audits. [The 340B Program] ensures patients with chronic conditions are staying on their medications, that we have a robust PrEP (Pre-Exposure Prophylaxis) program for preventing HIV and a drug delivery program. We can provide these to the communities that need them the most through the 340B Program. When we consider this change, and layer on the cashflow implication, the potential for denials, as well as the increased administrative costs to the manage the program, some of those wraparound services, those components by virtue of the funding through 340B, will start to shrink, and will be shifted to the administrative overhead.
Beth Feldpush: In the rebate model, each manufacturer can set up one program that they then work with, but hospitals must respond to all nine programs that manufacturers have put in place. I can't overstate enough, the administrative burden beyond that, beyond the very real tangible impact. I think this is a fundamental shift in handing over regulation of a federal program to an industry that has a financial stake in it. It really is the proverbial fox guarding the hen house here and it lines up with the pharmaceutical manufacturer's goal of killing the 340B program line by line -- death by a thousand cuts. It’s extremely concerning to see the program pivot in this manner.
Q: Is it realistic that this could be a one-year pilot?
Nicole Faucher: I think that it's certainly going to depend on the success factors of the pilot stage, but I do think rolling back a pilot of this size is going to be difficult. What makes this precedent is that the only manufacturers that are part of the pilot are those that are part of the IRA, but every covered entity that's a part of the 340B Program is a part of the pilot.
This is different from how most pilots are designed. There is usually an opt-in, or there is a benefit to being a part of a pilot, and in this case, that is not the design. The burden for the success of this program lies in the hands of the hospitals and covered entities that are most going to be impacted. They carry the burden of cost, operations and reconciliation. While there might be benefit to the improved transparency and visibility of the program, the burden of making the program successful relies on hospitals and covered entities that do not have the financial solvency to front the cost to run the program -- and they have no choice.
The administrative cost could be anywhere from a full-time employee or two all the way to over a half a million dollars a year. You compound that across all the participating hospitals, and it's going to cost health systems about $400 million a year of administrative costs to provide a pilot. The average DSH hospital is going to be floating about $72 million in cash to front the program. The real part that we're all working through is how do we best manage that and ensure it doesn’t impact the patients the program is intended to serve?
Q: What should hospitals and health systems be doing to prepare for the clinical, operational and financial impact of the Program?
Nicole Faucher: Hospitals and covered entities that are early in their pharmacy maturity have an opportunity to design their program with the rebates in mind. They can put a data infrastructure in place that will support the processes to include a look back and reconciliation process versus a front-end process. They will have an opportunity to start that design and governance from the beginning, and have options related to how they choose to sequence their growth.
For organizations like Grady Health System, with a highly established program, they will need to determine how to quantify their exposure in a compounding way. One of the most important things to do is to understand the quality of the data. Data, if properly assessed, can give valuable insight on NDC (National Drug Code) mappings, eligibility logic, risk related to managing denials, accumulator rules and the timing of the submission of claims. How a hospital and/or covered entity manages and reconciles the claims is going to impact the cashflows and amount of staff needed to oversee this work.
Testing vendor readiness, such as TPAs (Third Party Administrators) and wholesalers, is also going to be important. Vendors will be impacted by the pilot, and hospitals and covered entities will need to have a very tight understanding of the new integrations because they can introduce new risks. Every organization should also be revisiting their payer and manufacturer strategies to gauge if there are ways to improve engagement.
The 340B pilot is going to be very disruptive, so hospitals and covered entities will have to consider how to manage the changes, while setting up a strategy and needed operational workflows, and at the same time continue to function as an essential service line in the specialty pharmacy space.
Beth Feldpush: Hospitals and covered entities should be reaching out to Apexus, the prime vendor, HRSA, whether it's through the general email box or directly to the staff in the office of pharmaceutical affairs to ask these clinical, operational and financial questions. My hope is that they will offer further guidance. Everybody must be their own advocate in trying to seek out answers to these questions from the agency.
Q: What are the risks and mitigation strategies leaders should be considering and preparing for as we wait to see if the program takes effect this year?
Beth Feldpush: There is a tremendous risk with this data flow in that nothing precludes the manufacturers from using the data for other reasons. The data could also contain protected health information and therefore, there are HIPAA concerns. We need to get a better sense of this from Beacon and from the manufacturers.
The real risk is human risk. I'm very concerned about our hospital's ability to provide all of those services that they already don't receive a full direct reimbursement for, and if they are now more concerned about the cashflow issue, and whether they are even going to get the payments back. I'm concerned about the programs that our members offer because they really invest in improving their communities at large, not just patients’ health when they come into the four walls of the hospital but also promoting health out in the community.
Clearway Health: Pending a final ruling likely in the second quarter of 2026, we recommend continuing to prepare for the pilot program. This includes:
- Enrollment with Beacon, the technology platform operated by Second Site
- Ensuring that your data is complete, auditable and linkable
- Verifying that your systems can support retrospective rebate submission
- Coordinating across billing and claims operations
- Ensuring dispensing workflows support eligibility documentation
- Preparing for higher manufacturer audit volumes and deeper documentation needs
- Adjusting financial expectations for the shift from up-front discounts to delayed rebates
Clearway Health will continue to closely monitor developments and can help hospitals and covered entities plan and manage the changes from the 340B Rebate Model Pilot. For additional information, please contact us through our website here.



